THE NEWS
Evidence strongly supports immediate adoption of the CarePath system.
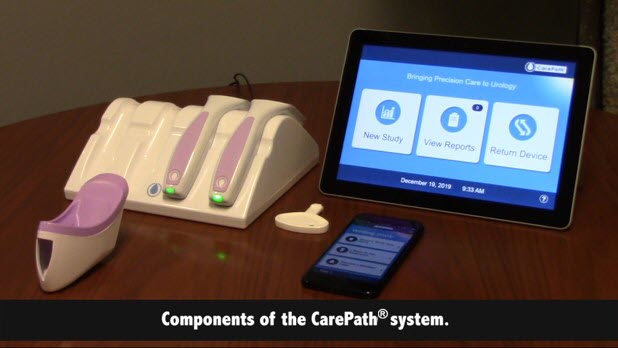
I-O Urology Launches First Complete Digital Diagnostic Platform for Remote Urologic Care
CarePath® technology increases engagement, improves compliance, and standardizes treatment pathways for patients with lower urinary tract symptoms.
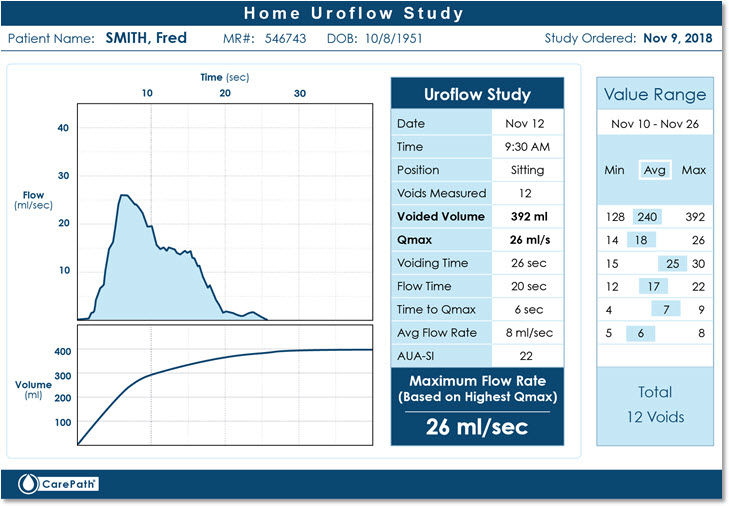
Uroflow Studies
In male patients with LUTS it is important to differentiate between bladder outlet obstruction symptoms secondary to benign BPH and other causes of bladder dysfunction. The value of routine uroflow studies in this population is clearly identified in the medical literature.
Journal of Clinical and Diagnostic Research. 2014 Apr, Vol-8(4): NC01-NC03
Sanjeev Singla(1), Ramneesh Garg(2), Ankit Singla(3), Sandeep Sharma(4), Jasdeep Singh(5), Pulkit Sethi
There was a positive correlation between peak flow rate, as was measured by uroflowmetry and lower urinary tract symptom severity.
The Urodynamic Evaluation of Lower Urinary Tract Symptoms in Men
Derek Griffiths, PhD, Paul Abrams, MD, Carlos A. D’Ancona, MD, Philip van Kerrebroeck, MD, Osamu Nishizawa, MD, Victor W. Nitti, MD, Foo Keong Tatt, MD, Andrea Tubaro, MD, Alan J. Wein, MD, Mo Belal, MD
Current Bladder Dysfunction Reports 2008, 3:49–57
Uroflow measurement is the least invasive urodynamic assessment. It gives an objective and quantitative indication of voiding dysfunction … for uroflowmetry to play a part in the diagnosis of BOO/BPO, the measurements need to be multiple.
Jean J. M. C. H. de la Rosette, Wim P. J. Witjes, Werner Schafer, Paul Abrams, Jenny L. Donovan, Tim J. Peters, Richard J. Millard, Cai Frimodt-Møller, Paraskevas Kalomiris, and the ICS – “BPH” Study Group; Neurourology and Urodynamics 17:99–108 (1998)
Department of Urology, University Hospital Nijmegen, Nijmegen, The Netherlands, Department of Urology, Universita¨ts Klinik Aachen, Aachen, Germany, Bristol Urological Institute, Southmead Hospital, Bristol, United Kingdom, Department of Social Medicine, University of Bristol, Bristol, United Kingdom, Department of Urology, Prince Henry Hospital, Little Bay, New South Wales, Australia, Department of Urology, Gentofte Hospital, University of Copenhagen, Hellerup, Denmark, Department of Urology, General Hospital of Sparta, Sparta, Greece
Despite the lack of evidence in the literature for close relationships between lower urinary tract symptoms and bladder outlet obstruction, the majority of urologists rely on symptomatology when selecting patients for prostatic surgery … There was little or no correlation between a wide range of symptoms and the results of free uroflowmetry and pressure and flow studies. From symptoms alone, it is not possible to diagnose bladder outlet obstruction. Pressure and flow studies and symptom profiles measure different aspects of the clinical condition that should be viewed separately in the evaluation and treatment decision of the patient presenting with lower urinary tract symptoms.
Stepan Vesely, Tomas Knutson, Magnus Fall, Jan-Erik Damber, and Christer Dahlstrand
Department of Urology, Sahlgrenska University Hospital, Goteborg, Neurourol. Urodynam. 22:301-305, 2003
These data indicate that IPS-score does not achieve sufficient diagnostic accuracy and its role in the assessment of BOO is limited. The grade of obstruction is more related to prostate volume, PVR, and maximum flow rate.
Symptoms and Diagnostics in Clinical BPH
M.D. Eckhardt Ph.D. Thesis, with summary in Dutch 2001; Utrecht University, The Netherlands
Flowmetry is a method of objectively assessing the voiding process. It is non-invasive, simple, and relatively inexpensive. Uroflowmetry measures a number of parameters of micturition, of which the most important is the maximum urinary free flow rate (Qmax.free)3. Because of the great intra-individual variability and the volume dependency of the Qmax.free, if possible, at least two flow rates, both with a volume ideally of >150 ml voided volume, should be obtained.
Ger E. P. M. van Venrooij, Harm H. E. van Melick, Mardy D. Eckhardt, and Tom A. Boon
UROLOGY 71 (3), 2008
Voiding data should have a prominent role in the initial evaluation of men with LUTS suggestive of BPH.
How to Make the Diagnosis of Benign Prostatic Disease
Mathias Maruschke, Chris Protzel, Oliver W. Hakenberg; Department of Urology, Rostock University, Rostock, Germany
European Urology Supplements 8 (2009) 490–4
The measurement of urinary flow rates is a urodynamic investigation. It assesses the combination of detrusor force and outflow opening and, thus, gives an indirect indication of these aspects of bladder function. Flow rates must be interpreted together with the voided volume. Low volumes give inaccurate flow-rate measurements. The most important parameter in men with LUTS is the maximum flow rate (Qmax); additional information is gained by looking at the voiding time and the flow pattern. It is mandatory to have more than one flow-rate measurement, as they can be variable (depending on voided volume, diurnal variation). The voided volume should be >150 ml.
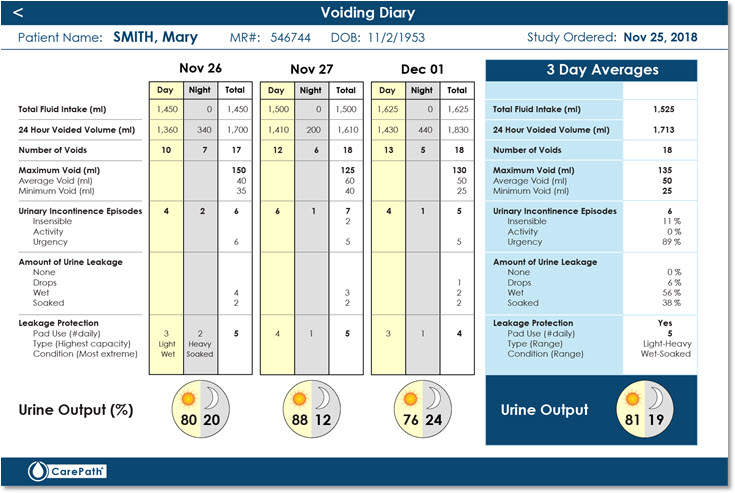
Voiding Diary Studies
Accepted as an essential investigation in the investigation and management of patients with lower urinary tract symptomatology (LUTS). In conditions such as nocturia they are the recognized “Standard of Care.” Their value in patients with bladder dysfunction is clearly shown in numerous published clinical articles.
Frequency volume charts should be used in men with lower urinary tract symptoms
International Journal of Surgery (2005) 3, 147-150; Prasanna Sooriakumaran, Christian Brown b, Mark Emberton
A frequency volume chart is a simple, easy-to-use, non-invasive tool that is useful in the assessment of patients with lower urinary tract symptoms. Though more sophisticated techniques are now available for diagnosis, the frequency volume chart should still be considered the first line investigation. In this review we summarize the indications and value of this age-old investigation. Urologists and primary care physicians should use the frequency volume chart more frequently in their practice.
J Reprod Med 1996;41:801–6.; Rabin JM, McNett J, Badlani GH.
In a study by Rabin et al, a computerized voiding diary was found to be associated with better patient compliance (in terms of a greater number of entries made) and increased patient preference than with a paper diary.
Developing and validating the International Consultation on Incontinence Questionnaire Bladder Diary. (requires MedScape subscription)
Euro Urol 2014;66:294–300.; Bright E, Cotterill N, Drake M, A
In total, 94% of patients found the electronic diary easy to use, there were no data errors, and the authors concluded that the real-time recordings obtained may have more accurately reflected patient symptoms.
Assessment of an electronic daily diary in patients with overactive bladder.
BJU Int 2003; 91:647–52.; Quinn P, Goka J, Richardson H.
This study shows that concerns about compliance with paper diaries are justified. Although patients reported high compliance, actual compliance was low and hoarding was common. The excellent compliance achieved with the electronic diary indicates that low compliance was not due to this particular sample or to an overly burdensome protocol. Overall, these results call into question the validity of paper diary records. Further, it demonstrated that compliance is often faked by subjects using paper diaries, giving the false impression of good compliance…. We confirmed that the electronic diary is a novel method of collecting clinically relevant symptom data from patients with an overactive bladder. In addition, the ease-of-use ratings support the use of the electronic diary as a superior alternative to paper diaries, providing real-time data which can be rapidly analysed, and thus allowing a speedy review of data during ongoing clinical studies.
Patient compliance with paper and electronic diaries
BMJ 2002;324:1193–4; Arthur A Stone, Saul Shiffman, Joseph E Schwartz, Joan E Broderick, Michael R Hufford
This study clearly demonstrates that relative to paper diaries, eDiaries can improve the scientific quality and integrity of PRO data. At a minimum, the eDiary, unlike paper diaries, allows for an evaluation of subjects’ compliance with the protocol. That is, automatic time-stamping in the eDiary, along with a variety of other compliance-enhancing features, can be used to evaluate and remediate when necessary to improve subject compliance. In contrast, prior paper methods do not allow for this compliance evaluation or remediation. In virtually all studies that implement paper diaries, the only measure of compliance is the submission of the diary card. But this offers no assurance that the diary was completed at the protocol-dictated time.
Urology 2004;64:966–969.; Ku J, Hong S, Kim H, Paick J-S, Lee S, Oh S-J.
Compared the International Prostate Symptom Score (IPSS) nocturia score and a 3-day FVC (frequency-volume chart) to assess the agreement as regards to the nocturia episodes. They found that a large number of subjects (67.7%) demonstrated a discrepancy between the number of nocturia episodes as assessed by FVC and IPSS nocturia index. They also found that overestimation of the nocturia episodes in the IPSS was more common than underestimation. Overestimation at the ICIQ-LUTS was a common finding when compared to ICIQ-BD … The findings of the present study revealed poor agreement between the subjectively estimated nocturnal frequency and chart-determined nocturnal frequency. Our results suggest that FV charts should be included as an integral part of evaluating nocturia in both sexes.
What is a clinician to do-believe the patient or her urinary diary?
Urology. 2003 Apr;61(4):802-9.; Kenton K1, Fitzgerald MP, Brubaker L.
Women with urge incontinence either overestimate or under record incontinence episode frequency in the urinary diary. This effect is more pronounced in women who are more bothered by incontinence.
Women overestimate daytime urinary frequency: the importance of the bladder diary
J Urol. 2009 May;181(5):2176-80; Stav K1, Dwyer PL, Rosamilia A.
Our results suggest that half of patients tend to overestimate daytime urinary frequency. However, the accuracy rate of nighttime frequency is much higher. A bladder diary provides invaluable information about urinary frequency and it should be an integral part of the routine assessment in women with lower urinary tract symptoms.
Voiding diaries: adherence in the clinical setting.
J Urol. 2005 Feb;173(2):487-9.; Pauls RN1, Hanson E, Crisp CC.
Although compliance with voiding diaries is reasonably high in the office setting, adherence to instructions is less optimal. Strategies to improve ease of use could benefit future patient care.
The need for voiding diaries in the evaluation of men with nocturia
JAOA • Vol 102 • No 5 • May 2002 • 261; Jamison S. Jaffe, Do; Phillip C. Ginsberg, Do; Daniel M. Silverberg, Md; Richard C. Harkaway, Md
The study findings suggest that voiding diaries are essential in helping to determine the actual number of voiding episodes per night and that the need for a voiding diary becomes more important as the perceived amount of nocturia increases.
Frequency Volume charts: An indispensable part of lower urinary tract assessment
Scandinavian journal of urology and nephrology, 179(179):47-53, February 1996; Abrams P, and Klevmark B
Frequency volume charts (FV charts) are widely used by those interested in lower urinary tract function … FV charts have an important role in objectively, recording patients’ symptoms, both as a base line and after therapeutic interventions. They are particularly important in everyday clinical use as a vital part of bladder training. In the research field they are important in providing objective evidence of changes in subjective symptoms in a treatment group as opposed to the placebo group. They have been particularly valuable in the evaluation of new drugs for the treatment of detrusor overactivity and benign prostatic obstruction. Most FV charts rely on pen and paper. However in the computer age the possibility of computerizing the FV chart is attractive.
European Urology 5 2 ( 2007) 811–8; Tet L. Yap, David A. Cromwell a, Christian Brown, Jan van der Meulen, Mark Emberton
Weak associations were found between the self-rated I-PSS scores and FV measures of voiding, suggesting that the accurate assessment of LUTS requires self-reported measures of symptoms and objective measures of voiding behavior.